“Blood Type and Health: Review How the ABO System Influences Disease ”

Tamara Ahmed Abd Alkareem1,a) mataz J. Jamai1,b), Mohammed Mahdi Sami1,C) and Aya zaid Mohammed1,d)
1Remote Sensing Department, College of Remote Sensing and Geophysics, Al-Karkh University of Science, Baghdad, Iraq
tamara1990@gmail.com
alwesy@kus.edu.iq
mohamedmahdi81@kus.edu.iq
28.Zaid@gmail.com
Abstract:
The ABO antigens found in human blood have different phenotypes and interact with cell physiology and disease via genetically produced glycoconjugate structures on the surface of RBC. Type O blood is more common in cases of cholera, plague, tuberculosis, mumps, high blood pressure, and cholesterol; type A blood is more common in cases of smallpox and Pseudomonas aeruginosa; and type O blood is the least likely to develop Type 2 Diabetes Mellitus (T2DM). Additionally, gonorrhoea, TB, Streptococcus and etc are more common in people with type B blood, whereas smallpox, E. coli, and salmonella are more common in those of type AB blood. Despite this, research has linked blood type B to a rise in TB as well as gonorrhoea cases. Blood types A and O have different infection rates when it comes to stomach cancer, according to research. In contrast to pancreatic cancer, infections to a greater extent in individuals with blood types A, B, and AB. In terms of susceptibility to breast cancer, blood type “A” stands out. The risk of breast cancer is lowest among those who blood type AB. Problems with Metabolism It is quite probable that blood types play a multifaceted function in metabolic disorders. Examining how different blood types are associated with the prevalence of different illnesses is the primary goal of this research.
Keywords: T2DM: Type 2 Diabetes Mellitus, RBC: Red Blood Cell
فصيلة الدم والصحة: مراجعة لكيفية تأثير نظام ABO على الأمراض
تماره احمد عبدالكريم ، معتز جليل جمعة، محمد مهدي سامي، اية زيد محمد
tamara1990@gmail.com
alwesy@kus.edu.iq
mohamedmahdi81@kus.edu.iq
28.Zaid@gmail.com
قسم التحسس النائي، كلية التحسس النائي والجيوفيزياء، جامعة الكرخ للعلوم
بغداد، العراق
الخلاصة:
مستضدات ABO الموجودة في دم الإنسان لها أنماط ظاهرية مختلفة وتتفاعل مع فسيولوجيا الخلية والأمراض من خلال هياكل الجليكوكونجوت المنتجة وراثيًا على سطح خلايا الدم الحمراء. الدم من النوع O أكثر شيوعًا في حالات الكوليرا والطاعون والسل والنكاف وارتفاع ضغط الدم والكوليسترول؛ الدم من النوع A أكثر شيوعًا في حالات الجدري والزائفة الزنجارية؛ والدم من النوع O هو الأقل عرضة للإصابة بمرض السكري من النوع 2 (T2DM). بالإضافة إلى ذلك، فإن السيلان والسل والمكورات العقدية وما إلى ذلك أكثر شيوعًا لدى الأشخاص الذين لديهم دم من النوع B، بينما الجدري والإشريكية القولونية والسالمونيلا أكثر شيوعًا لدى أولئك الذين لديهم دم من النوع AB. وعلى الرغم من ذلك، فقد ربطت الأبحاث فصيلة الدم B بارتفاع حالات السل وكذلك حالات السيلان. وفقًا للبحث، فإن فصائل الدم A وO لها معدلات إصابة مختلفة عندما يتعلق الأمر بسرطان المعدة. على عكس سرطان البنكرياس، تزداد الإصابة بالعدوى لدى أصحاب فصائل الدم A وB وAB. وتبرز فصيلة الدم “A” من حيث قابلية الإصابة بسرطان الثدي. ويكون خطر الإصابة بسرطان الثدي أقل لدى أصحاب فصيلة الدم AB. مشاكل الأيض: من المرجح أن تلعب فصائل الدم دورًا متعدد الجوانب في الاضطرابات الأيضية. ويهدف هذا البحث بشكل رئيسي إلى دراسة كيفية ارتباط فصائل الدم المختلفة بانتشار الأمراض المختلفة.
الكلمات المفتاحية: داء السكري من النوع الثاني (T2DM)، خلايا الدم الحمراء (RBC)
Introduction:
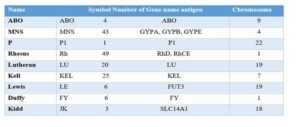
Red blood cell (RBC) antigens are part of the whole blood group system, which is regulated via a complex network of genes that may be either allele-specific or tightly linked on the same chromosome. Glycoconjugate structures on the surface of RBC, which are genetically generated and have an active involvement in both the physiology and pathophysiology of the cells, may take on different phenotypes when exposed to human ABO blood type antigens [1, 2]. In addition, the antigen-specific oligosaccharide structures are able to determine the blood type. So, major gene outputs include the glycosyltransferase enzymes that are useful link polysaccharide chain with sugar molecules, while secondary gene outputs include blood type antigens. When other people’s immune systems detect these carbohydrate components, they produce antibodies that target them [3]. The ABO blood type system has played a vital position within several illness report within the medical field [4]. Connections amongst ABO blood type as well as vulnerable for particular viral and noninfectious illnesses has been the subject of considerable debate, however, because of the lack of antibodies in some varieties of blood. Variations in the shape and function of blood membranes are a result of the turnout or obscurity of antigens in different blood types. It’s may be associated with health or disease depending on the functions that rely on the structure of blood types [1, 5]. Leukocytes, specific organs, plasma proteins, and platelets may also carry blood group antigens, in contrast to cell surface enzymes [6,7]. While most antigens are products of a single gene, changes in the genetic code can result in antigenic changes, new antigens [8]. These changes can be caused by deletions, inversions, insertions, alternative splicing. Although they were discovered initially, the ABO blood type antigens have since been the subject of much research and are hence likely the most important [9]. The glycoconjugate structures on red blood cells serve several purposes, such as receptors for external ligands, transporters, channels, structural proteins, adhesion molecules, enzymes, and viruses, bacteria, and parasites [10]. Our current understanding of the processes behind the connections amidst blood type antigens adhesion molecules is limited. Although it is easy to find a patient’s ABO blood type in their genetic composition, it has been correlated with several illnesses [11]. Worldwide, massive epidemiological investigations were conducted between 1960 and 1970 to test the widely claimed links between human ABO blood type and susceptibility to a variety of illnesses [12,13]. Several infectious diseases have been associated with ABO blood types [14], but noninfectious illness have not [15]. It is possible that environmental variables play a pivotal role in disease genesis, alongside host genetic factors. Numerous diseases, including gastric cancer and peptic ulcers, were investigated in regard to the ABO blood type system after Landsteiner’s discovery in 1901 [16,17]. It is believed that ABO antigens have had an evolutionary purpose by providing protection against infectious diseases [18].
Blood Groups:
Although it is easy to find a patient’s ABO blood type in their genetic composition, it has been associated with several illnesses [14]. Worldwide, massive epidemiological investigations were conducted between 1960 and 1970 to test the widely claimed links between human ABO blood type and susceptibility to a variety of illnesses [15]. Several infectious diseases have been associated with ABO blood types [7, 16], but noninfectious diseases have not [17]. It is possible that environmental variables play a pivotal role in disease genesis, alongside host genetic factors. Numerous diseases, including gastric cancer and peptic ulcers, were investigated in relation to the ABO blood type system after Landsteiner’s discovery in 1901 [18]. It is believed that ABO antigens have had an evolutionary purpose by providing protection against infectious diseases. On the other hand, ABO blood types have been associated with a higher risk of cancer, cardiovascular disease, infections, as well as haematologic disorders [19,20].
Any individual with a serum level of 6 months or more will have clinically significant levels of anti-A and/or anti-B antibodies, making ABO the most important factor in transfusions and transplants. Serum from blood kinds A and B can be found together, however serum from blood types O can only have antibodies to both A and B [25]. Antibodies in the recipient’s blood may be harmful to the administered blood during a blood transfusion if the recipient’s blood type is wrong. As an example, the recipient’s antibodies against type B blood will attack and kill when given type B blood if they have blood type A, as type A blood carries antibodies against type B blood [26]. The ABO antigens must be present before birth and must continue to be present throughout a person’s life. Babies begin producing their own ABO antibodies at three months of age, although they also begin to receive them from their mothers as they grow and mature. Rarely, erythroblastosis fetalis may be caused by an ABO incompatibility between the mother and the foetus. The mother’s immune system kills the baby’s red blood cells, leading to this kind of anaemia. This occurs most often when a woman has type O and her unborn child has type A or type B [25].
Classification of Blood Group: Rh (Rhesus) blood grouping is a technique that ranks red blood cells (RBCs) according to whether or not they carry the Rh antigen on their surface. Rh group antigen antibodies are associated with some of the most severe instances of haemolytic illness of the foetus and newborn (HDFN) and haemolytic transfusion responses. There are more than fifty red cell antigens in the Rh system, but the five most important ones are D, C, E, and e. The most serious problems that may arise from transfusions are associated with these five groups. 5. Transfusions of Rh-positive blood might cause complications for those who are Rh-negative due to an antigen deficit. The immune system responds to Rh incompatibility by producing anti-Rh antibodies, even if symptoms may not manifest initially. Repeated administration of Rh-positive blood that is incompatible with the body causes haemolysis because antibodies developed during the first transfusion target foreign red blood cells (RBCs), causing them to agglutinate.
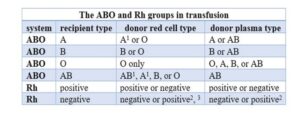
- No, in cases when the patient’s blood includes anti-A1 antibodies, which are specific to subgroup A individuals and their common type A red cells.
It’s not a good idea if the patient is a pregnant woman under the age of 45 unless there’s a life-threatening haemorrhage and transfusion of Rh-positive blood is really necessary.
3. Unless there are exceptional medical reasons, it is not possible if the patient’s serum includes anti-D, which an antibody against positive red cells is.
Association of ABO Blood Groups and Diseases:
Blood types in the context of sickness Hemostasis is significantly impacted by ABO blood types. Their quantitative impacts on von Will brand factor plasma levels are substantial, and factor VIII is no exception [19, 20]. Blood types A and AB are attached with an elevated danger of myocardial infarction, ischemic stroke, and venous thromboembolism, which may be explained by the regulation of thrombosis by functional ABO glycol transferases [21]. Non-O groups have been shown to have a greater risk of cerebral venous thrombosis.[22] There is evidence linking certain ABO blood types to an increased risk of preeclampsia; specifically, the AB blood type is linked to a 2.1-fold increased risk.[23]. Initial research suggested relate amidst the ABO system and cancer. Blood types A and B are positively associated with chronic hepatitis-B infection and pancreatic cancer, respectively, whereas blood types A and B are positively associated with ovarian cancer.[24] By decreasing rosette development, group O completes the safeguard against falciparum malaria. An Infection severity was increased in Vibrio cholera strains when blood group O was present. The most critical diseases are listed below. Blood type is correlated with elevated blood sugar, total cholesterol, as well as blood pressure, according to studies done on Iraqi patients. In contrast to pancreatic cancer, infections are more prevalent in people with blood types A, B, and AB. When it comes to breast cancer, blood type “AB” is the least common and blood type “A” is the most common. When it comes to metabolic diseases, the part played by different blood types is likely to be intricate. Nevertheless, we have discovered and given below several intriguing links. Blood pressure some studies found that those with blood type B had the highest prevalence of hypertension, whereas those with blood types A and AB had the lowest prevalence [25].
Infectious Diseases: When pathogens enter the body, they may cause a variety of symptoms that are known as infectious diseases. Parasites, viruses, bacteria, and fungus are the most common causes. Transmission of infectious diseases occurs most often via direct contact with infected individuals, contaminated food or drink, and insect bites. Infectious diseases can range from being relatively mild to life-threatening. Research in the literature has linked ABO polymorphism to certain infectious diseases [26]. Strong or weak barriers to infection are provided by the lack of A/B antigens and, by extension, anti-A/B antibodies. A large number of vertebrate species have benefitted from and support the ABO gene. On the other hand, it’s possible that anti-A/B antibodies may eventually disappear, therefore it might not matter whether popular within species A and B genes are functioning. However, a defense mechanism against pathogenic microbes may have evolved via the frequent A/B accuracy gene transformations that result in amino acid changes with inactive partial genes [27, 28].
Circulatory Diseases: There is strong evidence from several studies that people with blood types other than O are more likely to develop atherosclerosis and ischemic heart disease [29]. While heredity plays a significant role in CAD development, it also influences how individuals react to changes in risk variables. It’s increased avoidance of these glycoproteins, patients with blood type O have severe anemia due to a 25% reduction in plasma concentrations of clotting factors VWF and FVIII; this condition is linked to the H antigen associated with their spine [30]. Perinatal hemorrhage is known as preeclampsia. It is believed that the mother’s blood type is correlated with preeclampsia, one of the originating causes of parental as well as foetal mortality through pregnancy. An ABO blood type antigen’s beta-galactoses, including galactose, fucose, and N-acetyl-galactosamine, may be bound to by placental protein 13, also known as galectin-13. An further early indicator of preeclampsia is PP13. In primate species similar to humans, the placenta is responsible for producing PP13, which is then predominantly concentrated at the apical membrane of the syncytiotrophoblast and either released into the mother’s bloodstream or removed from it [31]. The same holds true for ABO and myocardial infarction [32].
Cancer: Malignancy progresses with disappearance of typical antigens and the acquisition of tumor antigens; the spreading potential of a tumor is indirectly proportional to the reduction in A, B, and H antigens [33]. There is a model that could explain the observed relationships between these markers’ presence or absence and disease outcomes [34,35]. Blood type A individuals do not perceive the A or “A-like” characteristics of these tumor antigens as alien, the higher cancer incidence in blood type A individuals compared to blood type O persons may be explained [38,39]. The ABO genotypes do show an increased risk of some cancers, it’s vital to remember that they don’t cause cancer per se, but rather signal a person’s sensitivity to particular diseases [41,42]. Many studies have failed to identify a relationship between blood type and breast cancer [43,44], indicating that absence of linkage does not give protection. Of all cancers, cancerous tumors kill more people than any other kind of cancer. When contrasted to those with blood type O, those with A, B, or AB have a 25% higher chance of having pancreatic and stomach cancers. Breast cancer is originate from a variety of sources, and the specific cells that undergo cancerous transformation determine the subtype of the disease. Breast cancer is most common in those with blood type “A,” whereas those with blood type “AB” are least likely to get the disease [57].
Hyperlipidemia: Hyperlipidemia and ABO blood type antigens have both been the subject of research. Researchers identified individuals whose blood types A and B had greater heights of total cholesterol, LDL cholesterol, and triglycerides and subordinate ranks of HDL cholesterol; however, those with blood type AB were protected against hyperlipidemia [60,61]. While some research has shown a integration of blood type A and elevated total and LDL cholesterol, no such correlation has been found between blood type A and HDL cholesterol [7, 58]. Intrinsic alkaline phosphatase (I-ALP) as well as apo lipoprotein B-48 (apo B-48) serum levels were shown to correlate with ABO as well as administrative assistant blood types, an intriguing discovery. I Blood type O and B administrative assistants, in comparison to A/AB secretors, non-secretors of all kinds, in addition to other blood types, had much greater serum levels of I-ALP and apo B-48. [62]. In addition to administrative assistants, blood type A has rather low activity relative to blood types B and O, and ABO no secretors alone have around 20% of the serum I-ALP of secretors [7]. It is thought that I-ALP is bound to ABO antigens on red blood cell (RBC) surfaces of non-secretors and is also taken up by secretors’ A antigens, which means it is excreted from circulation rapidly in these people. On the other hand, the soluble circulating antigens of O and B secretors bind to I-ALP in a way that prevents it from being removed in these people [60]. decreased serum apo B-48 levels are associated with decreased chylomicron production [61], probably lower serum cholesterol levels, and a genetic downregulation of I-ALP activity in the intestines in people with blood type A.
Diabetes Mellitus: According to many studies, those with blood type O are least likely to develop type 2 diabetes, while those with blood type B are most at risk, followed by those with blood types AB and A [62]. Blood type O was shown to be associated with increased blood sugar, total cholesterol, and blood pressure in Iraqi participants, whereas blood types A, B, and AB seemed linked with reduced risk or no risk at all [63]. However, a separate research out of Bangladesh found no correlation between ABO blood types and type 2 diabetes [64, 65].
Conclusion:
Individuals with predetermined genetic ABO blood types seemed correlated with an elevated danger of several pathogenic and nonpathogenic disorders, according to multiple research pertaining to the ABO phenotype .The filtering of human blood according to the genetic characteristics of red blood cells (RBCs) is known as the ABO blood typing system. Cholera, plague, and mumps are more common in people with blood type O, while smallpox is often seen in individuals with blood types A and AB. Tuberculosis is more common in people with blood types B and O. Blood types offer protection against certain diseases. People with blood type O are less likely to develop type 2 diabetes, while the opposite is true for blood types B, A, and AB. Regarding cancer, people with blood type A are more susceptible to stomach and breast cancer, while pancreatic cancer is more common in blood types A, B, and AB.
Acknowledgments:
This work would not have been possible without the financial as well as administrative backing of the Al-Karkh University of Science’s College of Remote Sensing & Geophysics and its Department of Remote Sensing.
References:
- Kabat, E. A. (2013). Blood group substances: their chemistry and immunochemistry. Elsevier.
- Franchini, M., & Liumbruno, G. M. (2013). ABO blood group: old dogma, new perspectives. Clinical Chemistry and Laboratory Medicine (CCLM), 51(8), 1545-1553.
- Wu, B. B., Gu, D. Z., Yu, J. N., Yang, J., & Shen, W. Q. (2020). Association between ABO blood groups and COVID-19 infection, severity and demise: A systematic review and meta-analysis. Infection, Genetics and Evolution, 84, 104485.
- Abegaz, S. B. (2021). Human ABO blood groups and their associations with different diseases. BioMed research international, 2021(1), 6629060.
- Ewald, D. R., & Sumner, S. C. (2016). Blood type biochemistry and human disease. Wiley Interdisciplinary Reviews: Systems Biology and Medicine, 8(6), 517-535.
- Ajmani, P. S. (2020). Immunohematology and blood banking: principles and practice. Springer Nature.
- Xie, N., Shen, G., Gao, W., Huang, Z., Huang, C., & Fu, L. (2023). Neoantigens: promising targets for cancer therapy. Signal transduction and targeted therapy, 8(1), 9.
- Li, J., Xiao, Z., Wang, D., Jia, L., Nie, S., Zeng, X., & Hu, W. (2023). The screening, identification, design and clinical application of tumor-specific neoantigens for TCR-T cells. Molecular Cancer, 22(1), 141.
- Foote, C. A., Soares, R. N., Ramirez‐Perez, F. I., Ghiarone, T., Aroor, A., Manrique‐Acevedo, C., … & Martinez‐Lemus, L. (2022). Endothelial glycocalyx. Comprehensive physiology, 12(4), 3781-3811.
- Ng, S. K. P. (2014). The Role of Distinct Host Glycans in the Evolution of Host Adapted Pathogens.
- Imran1&, M., Zia2&, R., Fareed3&, M. A., Javed1&, B., Ahsan4&, A., Jalil, K., … & Kalim10, Z. (2024). AJAB. Asian J Agric & Biol, (4).
- Rizzato, C., Kato, I., Plummer, M., Muñoz, N., Stein, A., Jan van Doorn, L., … & Canzian, F. (2013). Risk of advanced gastric precancerous lesions in Helicobacter pylori infected subjects is influenced by ABO blood group and cagA status. International journal of cancer, 133(2), 315-322.
- Rizzato, C., Kato, I., Plummer, M., Muñoz, N., Stein, A., Jan van Doorn, L., … & Canzian, F. (2013). Risk of advanced gastric precancerous lesions in Helicobacter pylori infected subjects is influenced by ABO blood group and cagA status. International journal of cancer, 133(2), 315-322.
- Moran, A. P., Gupta, A., & Joshi, L. (2011). Sweet-talk: role of host glycosylation in bacterial pathogenesis of the gastrointestinal tract. Gut, 60(10), 1412-1425.
- Rizzato, C., Kato, I., Plummer, M., Muñoz, N., Stein, A., Jan van Doorn, L., … & Canzian, F. (2013). Risk of advanced gastric precancerous lesions in Helicobacter pylori infected subjects is influenced by ABO blood group and cagA status. International journal of cancer, 133(2), 315-322.
- Arceci, R. (2006). Pediatric Oncology: A Comprehensive Guide. Springer Science & Business Media.
- Muehlenbein, M. P. (Ed.). (2010). Human evolutionary biology. Cambridge University Press.
- Cho, J., 2015. Gastrointestinal and hepatic manifestations of specific genetic disorders. Yamada’s Textbook of Gastroenterology, pp.2378-2398.
- Ginsburg, G. S., & Willard, H. F. (Eds.). (2009). Essentials of genomic and personalized medicine. Academic Press.
- Kupfer, S. S. (2022). Gastrointestinal and hepatic manifestations of specific genetic disorders. Yamada’s Textbook of Gastroenterology, 2205-2230.
- Hill, A. V. (2006). Aspects of genetic susceptibility to human infectious diseases. Rev. Genet., 40(1), 469-486.
- Yamamoto, F., Cid, E., Yamamoto, M., & Blancher, A. (2012). ABO research in the modern era of genomics. Transfusion medicine reviews, 26(2), 103-118.
- Yamamoto, F., Cid, E., Yamamoto, M., & Blancher, A. (2012). ABO research in the modern era of genomics. Transfusion medicine reviews, 26(2), 103-118.
- Lane, W. J., Westhoff, C. M., Gleadall, N. S., Aguad, M., Smeland-Wagman, R., Vege, S., … & Kong, S. W. (2018). Automated typing of red blood cell and platelet antigens: a whole-genome sequencing study. The Lancet Haematology, 5(6), e241-e251.
- Haji, H.M., 2022. Prevalence and Titre Levels of Anti-A and Anti-B Antibodies among Blood Group O Donors at Kenyatta National Hospital Blood Transfusion Unit, Kenya (Doctoral dissertation, JKUAT-COHES). http://localhost/xmlui/handle/123456789/5854.
- Gabaidze, S., Nagervadze, M., Akhvlediani, L., Nakashidze, N., Alfilo, A., Tsintsadze, I., Gorgadze, N., Khukhunaishvili, R., Koridze, M., Koiava, T. and Dolidze, K., 2023. ABO and Rh Blood Group Antigens and Natural Anti-A and ANTI-B Antibodies in the Neonates. WSEAS Transactions on Biology and Biomedicine, 20, pp.186-196. https://www.researchgate.net/publication/374639856.
- Shastry, S., Lewis, L.E. and Bhat, S.S., 2013. A rare case of haemolytic disease of newborn with Bombay phenotype mother. Asian journal of transfusion science, 7(2), p.153.doi: 10.4103/0973-6247.115583.
- Mitra, R., Mishra, N. and Rath, G.P., 2014. Blood groups systems. Indian journal of anaesthesia, 58(5), p.524.doi: 10.4103/0019-5049.144645.
- Daniels, G. and Reid, M.E., 2010. Blood groups: the past 50 years. Transfusion, 50(2), pp.281-289.https://doi.org/10.1111/j.1537-2995.2009.02456.x.
- Reid, M.E., Lomas-Francis, C. and Olsson, M.L., 2012. The blood group antigen factsbook. Academic press.
- Hamilton, J.R., 2019. Kidd blood group system: outwardly simple with hidden complexity. ISBT Science Series, 14(1), pp.3-8.https://doi.org/10.1111/voxs.12458.
- da Silva SF, Ferreira GM, Silva SL, et al. Red blood cell and leukocyte alloimmunization in patients awaiting kidney transplantation. Rev Bras Hematol Hemoter. 2013;35(3):185- 8. doi: https://doi.org/10.5581/1516-8484.20130043.
- Wang, Z., Liu, L., Ji, J., Zhang, J., Yan, M., Zhang, J., Liu, B., Zhu, Z. and Yu, Y., 2012. ABO blood group system and gastric cancer: a case-control study and meta-analysis. International journal of molecular sciences, 13(10), pp.13308-13321.https://doi.org/10.3390/ijms131013308.
- He, M., Wolpin, B., Rexrode, K., Manson, J.E., Rimm, E., Hu, F.B. and Qi, L., 2012. ABO blood group and risk of coronary heart disease in two prospective cohort studies. Arteriosclerosis, thrombosis, and vascular biology, 32(9), pp.2314-2320. https://doi.org/10.1161/ATVBAHA.112.248757.
- Khera, A.V. and Kathiresan, S., 2017. Genetics of coronary artery disease: discovery, biology and clinical translation. Nature Reviews Genetics, 18(6), pp.331-344. doi: 10.1038/nrg.2016.160.
- Zakai, N.A., Judd, S.E., Alexander, K., McClure, L.A., Kissela, B.M., Howard, G. and Cushman, M., 2014. ABO blood type and stroke risk: the REasons for Geographic And Racial Differences in Stroke Study. Journal of Thrombosis and Haemostasis, 12(4), pp.564-570.https://doi.org/10.1111/jth.12507.
- Lilova, Z., Hassan, F., Riaz, M., Ironside, J., Ken-Dror, G., Han, T. and Sharma, P., 2023. Blood group and ischemic stroke, myocardial infarction, and peripheral vascular disease: A meta-analysis of over 145,000 cases and 2,000,000 controls. Journal of Stroke and Cerebrovascular Diseases, 32(8), p.107215.https://doi.org/10.1016/j.jstrokecerebrovasdis.2023.107215.
- Lin, X.L., Zhou, B.Y., Li, S., Li, X.L., Luo, Z.R. and Li, J.J., 2017. Correlation of ABO blood groups with spontaneous recanalization in acute myocardial infarction. Scandinavian Cardiovascular Journal, 51(4), pp.217-220. https://doi.org/10.1080/14017431.2017.1312013.
- Carpeggiani, C., Coceani, M., Landi, P., Michelassi, C. and L’Abbate, A., 2010. ABO blood group alleles: A risk factor for coronary artery disease. An angiographic study. Atherosclerosis, 211(2), pp.461-466. https://doi.org/10.1016/j.atherosclerosis.2010.03.012.
- Avery P, Barzilai N, Benetos A, Bilianou H, Capri M, Caruso C, Franceschi C, Katsiki N, Mikhailidis DP, Panotopoulos G, Sikora E, Tzanetakou IP, Kolovou G: Ageing, longevity, exceptional longevity and related genetic and non-genetic markers: panel statement. Curr Vasc Pharmacol. 2014, 12: 662-673.
- Daniels, G., 2013. Knops blood group system and the Cost antigens. Human Blood Groups, 3rd edn (ed. by G. Daniels), pp.439-448. DOI:1002/9780470987018.
- Khalili, H., Wolpin, B.M., Huang, E.S., Giovannucci, E.L., Kraft, P., Fuchs, C.S. and Chan, A.T., 2011. ABO blood group and risk of colorectal cancer. Cancer epidemiology, biomarkers & prevention, 20(5), pp.1017-1020. https://doi.org/10.1158/1055-9965.EPI-10-1250.
- Henderson, J., Seagroatt, V. and Goldacre, M., 1993. Ovarian cancer and ABO blood groups. Journal of epidemiology and community health, 47(4), p.287. https://doi.org/10.1016/j.ejca.2010.08.009.
- Wolpin, B.M., Chan, A.T., Hartge, P., Chanock, S.J., Kraft, P., Hunter, D.J., Giovannucci, E.L. and Fuchs, C.S., 2009. ABO blood group and the risk of pancreatic cancer. Journal of the National Cancer Institute, 101(6), pp.424-431. https://doi.org/10.1093/jnci/djp020.
- Huang, J.Y., Wang, R., Gao, Y.T. and Yuan, J.M., 2017. ABO blood type and the risk of cancer–Findings from the Shanghai Cohort Study. PloS one, 12(9), p.e0184295. https://doi.org/10.1371/journal.pone.0184295.
- Hefazi, M., Litzow, M., Hogan, W., Gastineau, D., Jacob, E., Damlaj, M., Hashmi, S., Al‐Kali, A. and Patnaik, M.M., 2016. ABO blood group incompatibility as an adverse risk factor for outcomes in patients with myelodysplastic syndromes and acute myeloid leukemia undergoing HLA‐matched peripheral blood hematopoietic cell transplantation after reduced‐intensity conditioning. Transfusion, 56(2), pp.518-527. https://doi.org/10.1111/trf.1335.
- Vasan, S.K., Hwang, J., Rostgaard, K., Nyrén, O., Ullum, H., Pedersen, O.B., Erikstrup, C., Melbye, M., Hjalgrim, H., Pawitan, Y. and Edgren, G., 2016. ABO blood group and risk of cancer: A register-based cohort study of 1.6 million blood donors. Cancer epidemiology, 44, pp.40-43. https://doi.org/10.1016/j.canep.2016.06.005.
- Sun, W., Wen, C.P., Lin, J., Wen, C., Pu, X., Huang, M., Tsai, M.K., Tsao, C.K., Wu, X. and Chow, W.H., 2015. ABO blood types and cancer risk—a cohort study of 339,432 subjects in Taiwan. Cancer epidemiology, 39(2), pp.150-156. https://doi.org/10.1016/j.canep.2014.12.006.
- Hsiao, L.T., Liu, N.J., You, S.L. and Hwang, L.C., 2015. ABO blood group and the risk of cancer among middle‐aged people in T aiwan. Asia‐Pacific Journal of Clinical Oncology, 11(4), pp.e31-e36. https://doi.org/10.1111/ajco.12253.
- Huang, J.Y., Wang, R., Gao, Y.T. and Yuan, J.M., 2017. ABO blood type and the risk of cancer–Findings from the Shanghai Cohort Study. PloS one, 12(9), p.e0184295. https://doi.org/10.1371/journal.pone.0184295.
- Zhang, B.L., He, N., Huang, Y.B., Song, F.J. and Chen, K.X., 2014. ABO blood groups and risk of cancer: a systematic review and meta-analysis. Asian Pacific Journal of Cancer Prevention, 15(11), pp.4643-4650. DOI:http://dx.doi.org/10.7314/APJCP.2014.15.11.4643.
- MEZAAL, E.N., 2019. New method for the evaluation of propranolol with phosphotungstic acidvialong distance chasing photometer (NAG-ADF-300-2) using continuous flow injection analysis. International Journal of Pharmaceutical Research (09752366), 11(4). DOI: 10.31838/ijpr/2019.11.04.008.
- Sadiq, K.A., Mezaal, E.N. and Mohammed, M.A., 2023. Simultaneous spectrophotometric method for determination of both ciprofloxacin and cephalexin by using H-point standard addition method. Baghdad Science Journal. DOI: https://doi.org/10.21123/bsj.2023.8332.
- Naitza, S., Porcu, E., Steri, M., Taub, D. D., Mulas, A., Xiao, X., … & Cucca, F. (2012). A genome-wide association scan on the levels of markers of inflammation in Sardinians reveals associations that underpin its complex regulation. PLoS genetics, 8(1), e1002480.
- Mitra, R., Mishra, N., & Rath, G. P. (2014). Blood groups systems. Indian journal of anaesthesia, 58(5), 524-528.
- Pike, M. M., Larson, N. B., Wassel, C. L., Cohoon, K. P., Tsai, M. Y., Pankow, J. S., … & Bielinski, S. J. (2017). ABO blood group is associated with peripheral arterial disease in African Americans: The Multi-Ethnic Study of Atherosclerosis (MESA). Thrombosis research, 153, 1-6.
- Abd Alkareem, T., Hassan, S., & Abdalhadi, S. (2023). Breast Cancer: Symptoms, Causes, and Treatment by Metal Complexes: A Review. Advanced Journal of Chemistry-Section B: Natural Products and Medical Chemistry, 5(4), 306-319.
- Günaydın, Z. Y., & Yılmaz, E. (2023). The association between ABO blood groups and TASC II classification in patients with peripheral artery disease. Vascular, 31(3), 467-472.
- Turkey, N. S., & Mezaal, E. N. (2020). Continuous flow injection analysis, turbidmetric and photometric determination of methyldopa drugs using a new long distance chasing photometer (NAG-ADF-300-2). Indian Journal of Forensic Medicine & Toxicology, 14(4), 1495.
- Mezaal, E. N., & Turkey, N. S. (2020). Assessment of Long Distance Chasing Photometer (NAG-ADF-300-2) by Estimating the Drug Atenolol with Povidone Iodine Via CFIA. Ibn AL-Haitham Journal For Pure and Applied Science, 33(1), 65-83.
- Mohammed, M. A., & Sadiq, K. A. (2023). Simple Spectrophotometric Method for Determination of Drug Lisinopril in Pure Form and Pharmaceutical Formulations.
- Al-Rubaei, Z. M., Alubaidi, G. H., & Alubaidi, T. A. Kinetic Study of the Effect Some Novel Lipid Lowering Compounds on Creatine Kinase and 3-Hydroxy-3-Methy-Glutaryl-CoA Reductase Activities.
- Tekeste, Z., & Petros, B. (2010). The ABO blood group and Plasmodium falciparum malaria in Awash, Metehara and Ziway areas, Ethiopia. Malaria journal, 9, 1-4.
- Koley, S. (2008). The distribution of the ABO blood types in patients with diabetes mellitus. The Anthropologist, 10(2), 129-132.
- Öner, C., Doğan, B., Telatar, B., Çelik Yağan, C.F. and Oğuz, A., 2016. Frequency of ABO/Rhesus blood groups in patients with diabetes mellitus.